Retinal detachment is a condition where the retina, which lines the inner surface of the eye, separates from the underlying layer (the retinal pigment epithelium) and peels away.
The retina functions like the film in a camera, receiving light and transmitting visual information to the brain.
If the retina detaches from its position, the supply of oxygen and nutrients is cut off, damaging retinal cells.
If left untreated, this can lead to permanent vision loss.
Types of Retinal Detachment
This is the most common type, accounting for approximately 90% of all retinal detachments.
A hole (tear) or tear forms in the retina, allowing vitreous fluid to enter through the opening and lift the retina. The primary causes include vitreous degeneration due to aging, high myopia, and trauma.

Fibrous membranes or scar tissue forming on the retinal surface pull on the retina, causing it to detach.
This condition primarily occurs in cases of diabetic retinopathy, retinal vascular occlusion, intraocular inflammation, and post-traumatic complications.
It occurs when fluid accumulates beneath the retina without any retinal holes or traction.
Causes may include inflammation of the retina or choroid, tumors, severe hypertension,
or preeclampsia.
Symptoms of retinal detachment
Retinal detachment may present with few or mild symptoms in its early stages,
but as the condition progresses, the following symptoms may appear:

When retinal detachment occurs, you may see small spots or
flashes of light like sparks floating in front of your eyes.

Part of the retina may detach,
causing blurred vision
or the appearance of shadow-like areas in your field of vision.
Straight lines may appear curved, or objects
may appear distorted.

Floaters, threads,
and spiderweb-like patterns suddenly increase in your field of vision.

Partial vision loss in one eye may occur gradually,
or the field of vision may narrow like a tunnel.

When the detached retina invades the macula,
the area you want to see becomes blurry.

Retinal Detachment Self-Check
If any of the following apply to you, visit an ophthalmologist.
✔ Floating spots or thread-like objects suddenly increased significantly.
✔ Even with your eyes closed, it looks like light is flashing.
✔ It feels like a black shadow or curtain is falling over the edges of my vision.
✔ Vision suddenly becomes blurry or deteriorates
✔ I recently experienced a strong impact to my eye.

Causes of Retinal Detachment
Posterior vitreous detachment
As we age, the vitreous gel filling the eye shrinks and pulls away from the retina.
This pulling action can create holes or tears in the retina. The incidence increases after age 50.
High myopia
The more severe the myopia, the longer the eyeball becomes and the thinner the retina, making it more prone to developing holes.
Patients with high myopia have a high risk of
retinal detachment even at a young age.
Eye injury
If the eye receives a strong impact from a ball or fist, a traffic
accident, a fall, or similar causes,
damage to the retina may occur.
After cataract surgery
Vitreous changes are accelerated after cataract surgery, slightly increasing the risk of retinal detachment.
Regular follow-up examinations after surgery are important.
Previous history of retinal detachment
If retinal detachment occurs in one eye,
it is known that there is approximately a 10% chance it will also occur in the other eye.
Diabetes
Diabetic retinopathy can cause
scarring on the retina,
which may lead to retinal detachment.

Retinal Detachment Diagnosis/Examination
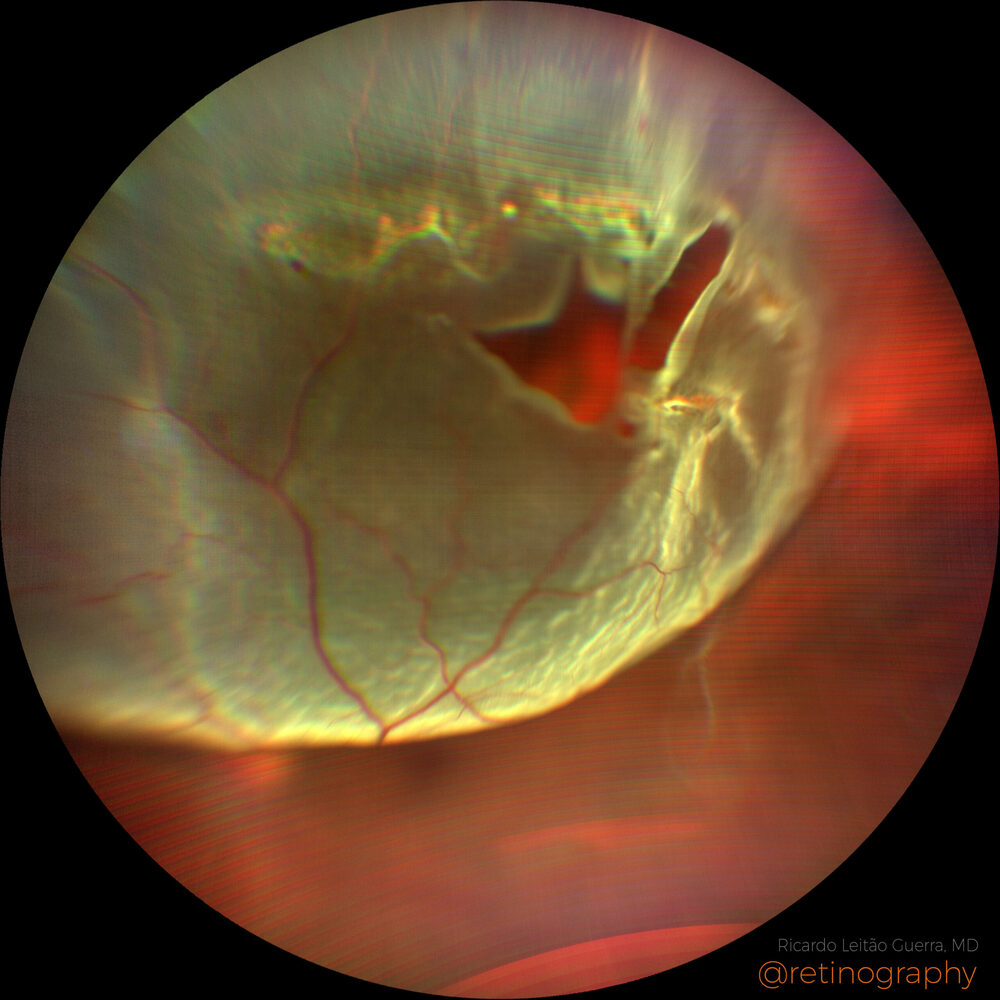
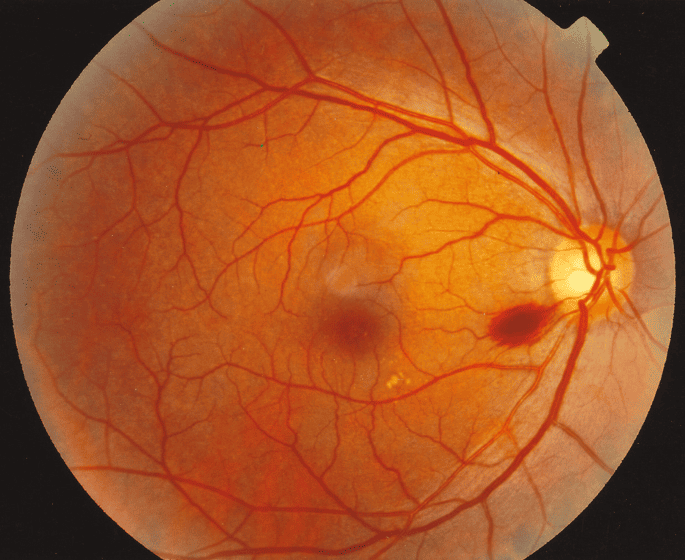
Fundus Examination
After dilating the pupils, the entire retina is examined using a special lens.
This is the most fundamental examination that allows direct observation of retinal tears,
the extent of detachment, and the condition of the vitreous.
Fundus photography
Retinal photographs are taken to document the location and extent of lesions.
Wide-angle fundus photography allows for broad examination
of the peripheral retina.
Ultrasound examination
When the fundus is difficult to visualize due to vitreous hemorrhage, ultrasound is used to assess the condition of the retina.
It can determine whether the retina is attached or
detached.
Prevention Guidelines for Retinal Detachment

Wear protective eyewear during strenuous exercise or work to prevent eye injuries.
Particular caution is needed if you have high myopia.
We effectively manage systemic diseases such as diabetes and hypertension that affect retinal health.

High-risk groups (those with high myopia, a family history of retinal detachment, a history of cataract surgery, diabetes, etc.)
should undergo regular dilated fundus examinations to detect retinal tears or degeneration early.
Retinal detachment is an ophthalmic emergency. If the macula is still attached, undergoing surgery within 24 to 72 hours is crucial for preserving vision.
Even if the detachment extends to the macula, prompt treatment significantly improves the chances of recovery.
Yes, if retinal detachment occurs in one eye, the risk of it happening in the other eye also increases by about 10%.
Both eyes should undergo regular checkups, and if a hole or degeneration is found in the other eye, consider preventive treatment.
High myopia is a major risk factor for retinal detachment. Get dilated fundus examinations at least once a year, and visit an ophthalmologist immediately if you experience abnormal symptoms such as increased floaters or photopsia. It is advisable to avoid sports involving intense impact.
LASIK, LASEK, and other corneal refractive surgeries themselves do not cause retinal detachment.
However, most people who undergo these surgeries have myopia, and high myopia itself is a risk factor for retinal detachment, so regular check-ups are necessary.