Diabetic retinopathy is a complication of diabetes that causes damage to the tiny blood vessels in the retina, leading to vision loss.
Persistently high blood sugar weakens the small blood vessels supplying oxygen and nutrients to the retina,
leading to bleeding or swelling that affects vision.
In the early stages, there are often few noticeable symptoms, so it frequently progresses unnoticed.
Types of Diabetic Retinopathy
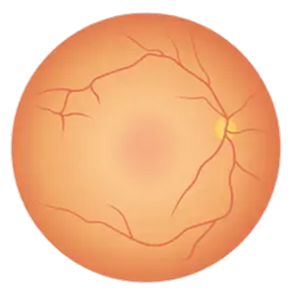
In the early stage, the retinal microvasculature weakens, leading to microbleeds, exudates, and microaneurysms.
It is classified into mild, moderate, and severe stages, with the severe nonproliferative stage carrying a high risk of progression to the proliferative stage.
As symptoms are often absent, regular check-ups are crucial.
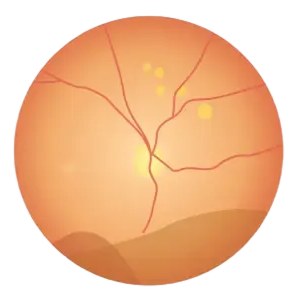
Damaged blood vessels send signals of oxygen deprivation, causing abnormal new blood vessels to grow.
These new blood vessels are extremely fragile and prone to bleeding, which can lead to vitreous hemorrhage or retinal detachment, causing sudden vision loss.
Symptoms of Diabetic Retinopathy
Diabetic retinopathy often has no noticeable symptoms in its early stages.
By the time symptoms appear, the condition may already be quite advanced.
Therefore, regular eye exams are essential for all diabetes patients, regardless of whether symptoms are present.

You may see spots, threads, or cobweb-like things floating in your vision. This could be an early sign of vitreous hemorrhage.

Your vision fluctuates or appears blurry, as if everything is covered in fog. Vision can change along with blood sugar fluctuations.

It may appear faded, or
color differentiation becomes more difficult than before.

It becomes difficult to distinguish objects in dark environments, and adaptation slows when moving from bright to dark areas.

When macular edema is present, central vision may become blurred, or depending on the location of the hemorrhage, part of the visual field may appear obscured.

If vitreous hemorrhage or retinal detachment occurs,
your vision may suddenly darken partially or completely.
This is an emergency situation, so you must visit the hospital immediately.

Diabetic Retinopathy Self-Check
Diabetic retinopathy is difficult to self-diagnose, so it is important to undergo regular eye examinations.
However, if you experience any of the following symptoms, you must visit an ophthalmologist:
✔️ Floating spots or streaks in your vision
✔️ Blurring or distortion in the center of vision
✔️ Vision deteriorates rapidly
✔️ Vision deteriorates rapidly in dark environments

Causes of Diabetic Retinopathy
Prolonged hyperglycemia
Persistently high blood sugar levels
damage the walls of the retina's tiny blood vessels,
causing them to become blocked or leak.
Duration of diabetes
The longer the duration of diabetes, the higher the likelihood of developing retinopathy.
After 15 to 20 years following a diabetes diagnosis, some degree of retinal changes is observed in most patients.
Poor blood pressure control
High blood pressure places additional pressure on already weakened retinal blood vessels, worsening the damage.
This is why managing blood pressure is just as important as managing blood sugar.
Dyslipidemia
High cholesterol and triglyceride levels
damage vascular health and promote the accumulation of exudates within the retina.
Kidney disease
신장 기능이 나쁘거나 신장 질환이 있는
경우, 당뇨 망막병증 발생 위험이 높아질 수 있습니다.
Genetic factors
If you have poor kidney function or kidney disease,
the risk of developing diabetic retinopathy may increase.

Diagnosis/Examination of Diabetic Retinopathy
After dilating the pupils, examine the retinal vessels and periphery.
Fundus examination, optical coherence tomography (OCT), retinal angiography, and other detailed examinations

Treatment for Diabetic Retinopathy
Medical Management of Diabetes
Intraocular antibody injection
Retinal laser treatment
Surgical treatment
Prevention Guidelines for Diabetic Retinopathy

Smoking accelerates blood vessel damage, so you must quit smoking.
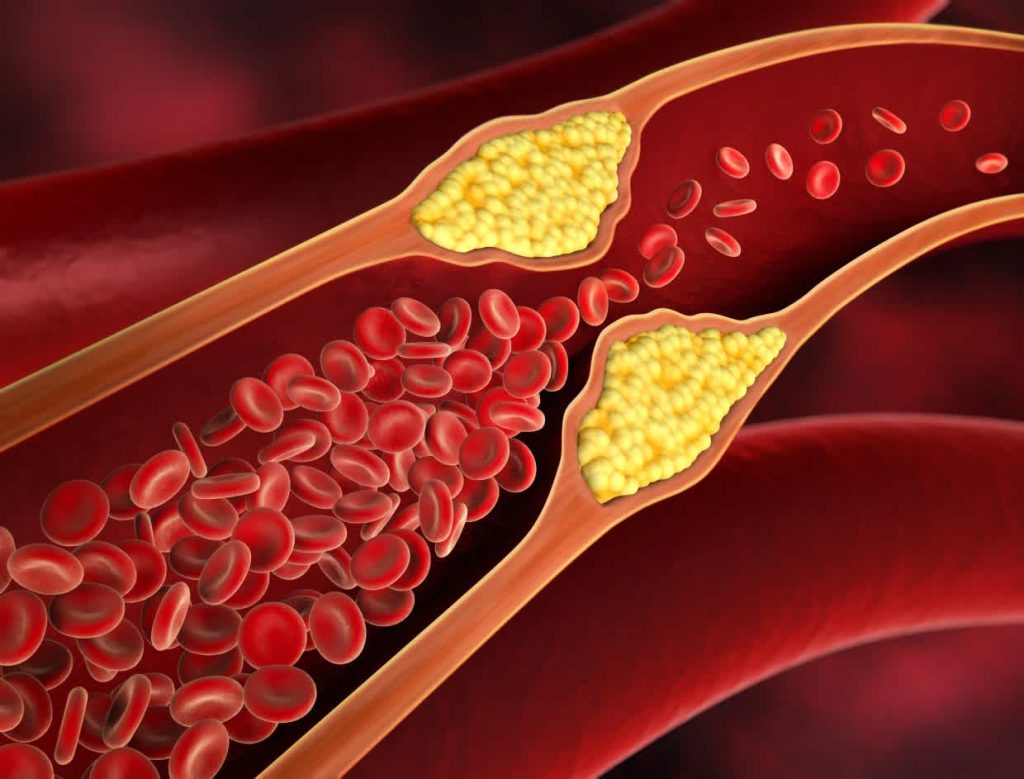
If you have dyslipidemia, actively treat it to maintain vascular health.
Maintain target blood pressure (typically below 130/80 mmHg) to reduce the strain on the retinal blood vessels.

당화혈색소(HbA1c)를 목표 범위 내로 유지하는 것이 가장 중요합니다.
혈당 조절이 잘 되면 망막병증 발생과 진행을 크게 늦출 수 있습니다.
Not all diabetes patients develop retinopathy. However, the risk increases with the duration of the disease.
Proper management of blood sugar, blood pressure, and cholesterol can significantly prevent its onset and progression.
After being diagnosed with diabetes, you should have your first eye exam within five years, followed by regular eye exams thereafter.
If you have had diabetes for a long time, you should have exams more frequently.
To prevent diabetic retinopathy, blood sugar management is most important.
Additionally, regular eye exams and management of conditions such as high blood pressure and high cholesterol are necessary.
It usually affects both eyes, but the degree of progression may differ between them.
If detected in one eye, the other eye should be carefully monitored.