Keratitis is a condition where inflammation occurs in the cornea, the transparent outer layer of the eye. The cornea is a crucial part that allows light to pass through and determines vision.
If damaged, it can lead not only to pain but also to decreased vision and even permanent vision loss.
Keratitis is classified as infectious or non-infectious based on its cause. Particularly if treatment is delayed, it can progress to corneal opacity, ulceration, and blindness,
making early diagnosis and prompt treatment extremely important.
Symptoms of Keratitis
Symptoms of keratitis vary depending on the cause and severity, but commonly include pain, redness, and decreased vision.
Symptoms can progress rapidly, requiring careful attention.
Pain manifests in various forms:
stabbing, burning, throbbing.

The whites of the eyes become red and inflamed,
especially around the edge of the cornea (limbus).
This is prominent in pan-uveitis.

Corneal opacity or edema causes blurred vision. When the central cornea is affected, severe vision loss occurs.
I've become extremely sensitive to light,
making it difficult to open my eyes in bright places.

I keep feeling like something is in my eye.

A white or grayish cloudy area may be visible on the cornea. If you see a white spot or film over the black pupil when looking in a mirror, you should suspect keratitis.
.

Causes of Keratitis
bacteria
Infections are primarily caused by Staphylococcus aureus or Pseudomonas aeruginosa,
and improper contact lens management (prolonged wear, inadequate disinfection) is a major risk factor.
Virus
Herpes simplex virus (HSV) is the most common cause. It is highly recurrent, and the varicella-zoster virus can also be a cause.
Eye injury
Corneal abrasions, foreign bodies, chemical substances, ultraviolet exposure, and plant-related trauma (during agricultural work) are causes of keratitis.
Dry eye syndrome
When the protective function of the corneal surface is impaired due to insufficient tears,
it becomes vulnerable to infection and inflammation.
Eyelid abnormality
In cases where the eyelid does not close completely (ptosis, facial nerve paralysis, thyroid eye disease),
or when eyelashes prick the eye (trichiasis), corneal damage may occur.
Contact lens use
It occurs due to prolonged wear, poor hygiene management,
or sleeping while wearing lenses.
Prevention Guidelines for Keratitis
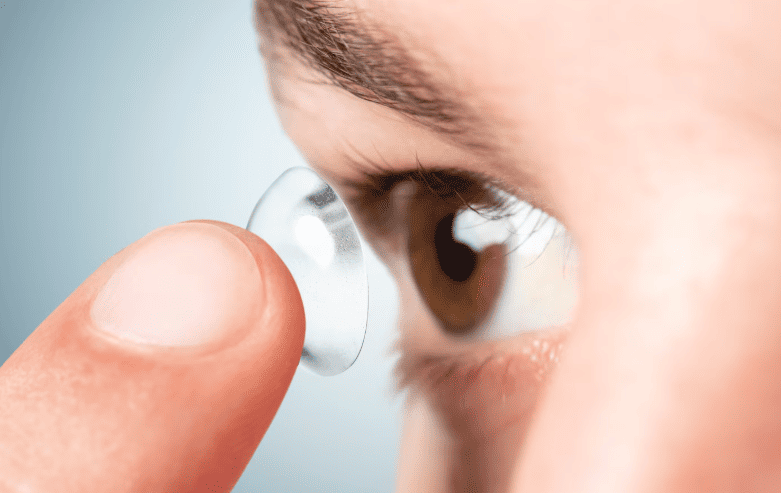
Follow the recommended wearing time and never sleep with your lenses in.
Rinse the case daily with solution, air-dry it, and replace it every three months.

Germs or viruses on your hands can get into your eyes.

Wear protective eyewear during work activities (welding, grinding, farming, gardening, etc.).
Use protective equipment during sports activities as well.
Conjunctivitis is an inflammation of the conjunctiva covering the white part of the eye, with redness and discharge as the main symptoms, but it usually does not affect vision.
Keratitis is an inflammation of the transparent cornea covering the black pupil, accompanied by severe pain, sensitivity to light, and decreased vision; if left untreated, it can lead to blindness.
Keratitis is a much more serious condition.
Viral keratitis (adenovirus, herpes) is contagious, so avoid sharing towels, pillows, etc., and practice thorough hand hygiene.
Bacterial, fungal, and Acanthamoeba keratitis are not transmitted through ordinary contact.
Never add medication arbitrarily. Steroid eye drops, in particular, can rapidly worsen herpes keratitis or fungal keratitis.
Treatment varies completely depending on the cause, so you must use only the medication prescribed after an ophthalmologist's examination.
You must stop wearing contact lenses until the keratitis is completely cured. Discard the lenses and case used during the infection and replace them with new ones.